Intracytoplasmic Sperm Injection (ICSI) has become a groundbreaking treatment in assisted reproductive technology (ART), offering hope to many couples struggling with infertility. ICSI is a type of in vitro fertilization (IVF) that involves the direct injection of a single sperm into an egg, bypassing many of the natural barriers to fertilization. While ICSI has significantly improved the chances of conception for couples facing male infertility or other fertility challenges, success rates can vary widely based on a number of factors. This blog delves into the success rates of ICSI, the key factors that influence these outcomes, and what couples can do to optimize their chances of a successful pregnancy.
What is ICSI?
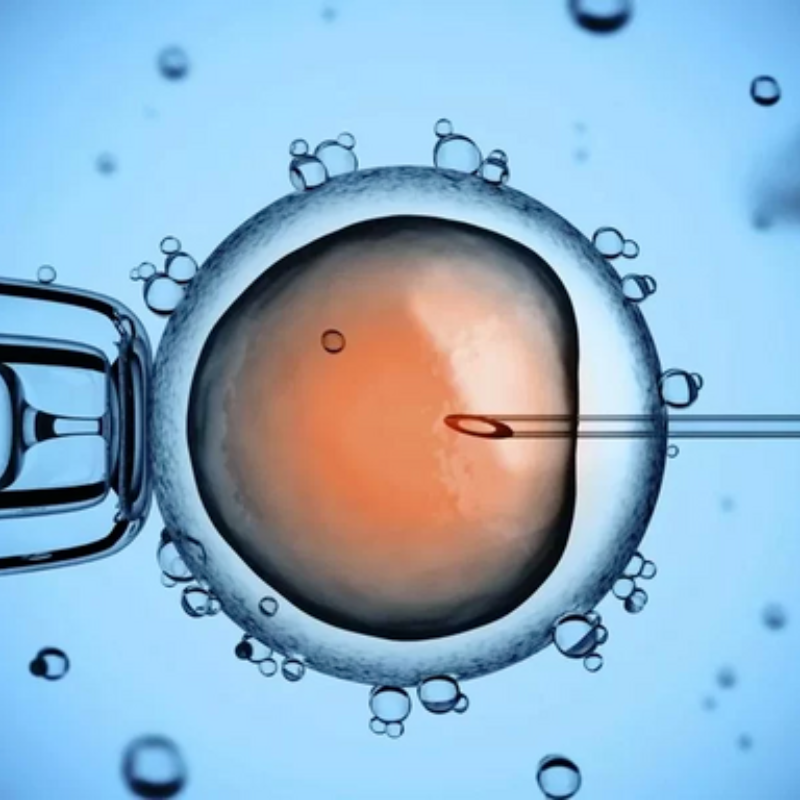
ICSI is a specialized form of IVF that was developed to address male infertility issues, particularly those related to sperm quality or quantity. In a standard IVF procedure, eggs are retrieved ICSI from the woman and fertilized in a laboratory dish with sperm. However, in cases of severe male infertility—such as low sperm count, poor sperm motility, or abnormal sperm morphology—traditional IVF may not be effective. ICSI, on the other hand, involves injecting a single sperm directly into an egg using a fine needle, overcoming the need for sperm to penetrate the egg’s protective layers on their own.
ICSI is also used in cases where there are issues like poor egg quality, previous IVF failures, or when sperm collection from the male partner is difficult or limited. The procedure has revolutionized infertility treatment by providing a solution for couples facing male-related fertility problems and significantly improving fertilization rates.
The general Success Rates of ICSI
The success of ICSI varies depending on a range of factors, but in general, ICSI has a high success rate, comparable to that of traditional IVF. According to data from fertility clinics and research studies, the average success rate of ICSI ranges from 30% to 40% per cycle, with live birth rates ranging from 20% to 35%. However, these statistics are averages, and success rates can vary significantly based on individual circumstances.
Key Factors That Influence the Success Rates of ICSI
Age of the Woman
One of the most significant factors influencing the success rates of ICSI is the age of the woman undergoing the procedure. As women age, the quantity and quality of their eggs decline, which can negatively affect the chances of successful fertilization and pregnancy. For women under 35, ICSI success rates tend to be higher, with the likelihood of achieving a live birth being around 40% to 50% per cycle. However, for women over the age of 40, success rates decrease significantly, with live birth rates dropping to around 10% to 20%.
Egg quality and the ovarian reserve (the number of viable eggs available for fertilization) are major considerations in this context. As women age, their eggs may have more chromosomal abnormalities, which can lower the chances of a successful pregnancy.
Sperm Quality and Quantity
Since ICSI directly involves sperm injection into the egg, the quality and quantity of sperm play a crucial role in the procedure’s success. Sperm characteristics, including motility (the ability to swim), morphology (shape), and concentration, are assessed before the procedure to determine if ICSI is necessary. If sperm quality is poor, the chances of successful fertilization using ICSI are lower.
Furthermore, sperm retrieved from men with genetic conditions or severe motility issues may have a lower chance of successfully fertilizing the egg and leading to a healthy embryo. Advances in sperm selection techniques, such as ICSI using sperm retrieved from testicular tissue in cases of azoospermia (absence of sperm in semen), have improved success rates for men with more severe fertility problems.
Embryo Quality and Development
The quality of the embryos that result from ICSI is another key factor in determining the chances of success. After fertilization, the embryos are monitored for their development, and those that are of higher quality have a better chance of implanting successfully in the uterus. Embryo quality is influenced by the health of both the eggs and the sperm, and advanced techniques like genetic screening of embryos (PGT-A) can help select the healthiest embryos for transfer.
Embryo culture conditions also impact success rates. The environment in which the embryos are cultured (temperature, pH, and nutrient levels) can affect their development, and the use of state-of-the-art laboratory equipment helps ensure the highest chances of healthy embryo formation.
Ovarian Reserve and Egg Quality
The woman’s ovarian reserve, which refers to the quantity and quality of her eggs, is closely linked to her age and overall fertility health. A diminished ovarian reserve can lead to lower quality eggs and a reduced likelihood of successful fertilization and embryo development. Women with a high ovarian reserve, typically under the age of 35, are more likely to have multiple embryos available for transfer, increasing the chances of a successful pregnancy.
Couples with diminished ovarian reserve may still have success with ICSI, but the success rate may be lower, and additional interventions like egg donation or the use of frozen embryos may be considered.
Uterine Health and Endometrial Quality
A woman’s uterine environment is essential for the successful implantation of embryos. Even if the embryos are healthy and well-developed, a suboptimal uterine environment can hinder implantation. Factors such as endometrial thickness, the presence of fibroids, polyps, or scarring, and overall uterine health can affect the chances of success with ICSI.
Women with a healthy uterus, with no significant abnormalities, tend to have better outcomes. In contrast, women with conditions like polycystic ovary syndrome (PCOS), endometriosis, or uterine abnormalities may experience lower success rates.
Previous Fertility History
A woman’s previous fertility history also plays a role in ICSI outcomes. For example, women who have experienced previous IVF or ICSI failures, recurrent miscarriages, or other fertility challenges may have lower chances of success. However, the presence of these factors does not necessarily rule out success, as many women who have had prior challenges eventually achieve pregnancy through ICSI.
Fertility specialists may recommend additional tests, such as genetic screening or immunological tests, to identify any underlying factors that could impact success.
Lifestyle Factors
Lifestyle choices can have a significant impact on fertility outcomes. Smoking, excessive alcohol consumption, poor diet, and lack of exercise can all lower the chances of a successful pregnancy through ICSI. Couples undergoing ICSI are advised to adopt healthier lifestyles by quitting smoking, reducing alcohol intake, maintaining a balanced diet, and engaging in regular exercise to improve overall health and fertility.
Stress and mental health also play a role in fertility outcomes. Couples undergoing fertility treatments should consider counseling or support groups to help manage the emotional challenges associated with the process.
Optimizing Your Chances of Success with ICSI
Choosing the right Fertility Clinic
Selecting a fertility clinic with experience and success in ICSI procedures is essential. It’s important to research the clinic’s success rates, patient reviews, and the qualifications of its medical team. A clinic that uses advanced technologies and offers personalized care can greatly improve your chances of success.
Genetic Screening and Counseling
For couples with known fertility challenges or genetic issues, genetic screening of embryos (PGT-A) can help identify the healthiest embryos for transfer. This technique can improve success rates and reduce the risk of miscarriage, particularly for women of advanced maternal age.
Mental and Emotional Support
Undergoing ICSI can be an emotionally and physically draining process. Couples are encouraged to seek emotional support through counseling, stress-management techniques, and connecting with others who have undergone similar treatments. Managing stress and maintaining emotional well-being can positively influence the success of fertility treatments.
Conclusion: Navigating the Journey of ICSI
The success rates of ICSI are influenced by various factors, including the age and health of the woman, sperm quality, embryo quality, and lifestyle choices. While ICSI offers hope to couples facing infertility, especially male infertility, it’s important to understand that success is not guaranteed. By working closely with a fertility specialist, addressing any underlying health conditions, and maintaining a healthy lifestyle, couples can optimize their chances of a successful outcome. With ongoing advancements in fertility technology, ICSI continues to offer a path to parenthood for many individuals and couples worldwide.